Researched and written by Jennifer Coates
The Anatomy of the brain and the science of CTE
When you hear these 3 letters ‘CTE’ you will more than likely think of the scandal that stole the headlines in America for several years, where there was a huge amount of publicity surrounding many ex NFL American footballers who were involved in violent crime and a spate of violent suicides, Aaron Hernandez being the most famous of these cases after he killed 3 people and then committed suicide in Prison. Then there was the infamous huge litigation against the NFL, where more than 4,500 athletes took the NFL to court for concealing the dangers of concussions impact on brain long-term health, they settled out of court in 2013 with a staggering $765m settlement, but still would not accept liability.
There is currently a similar case in the UK against various rugby union, rugby league and football governing bodies, with over 1000 claimants seeking compensation for their alleged failure to inform and protect their players of their long-term risks to their brains from playing these sports, with high profile international athletes such as Steve Thompson MBE and Alix Popham being diagnosed with probable CTE and early on-set dementia. But what exactly is CTE?
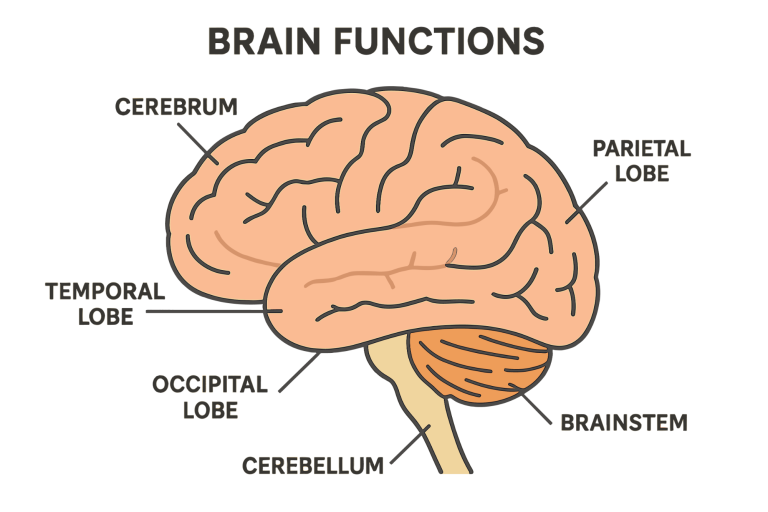
Before we talk about how CTE effects the human brain it is important to understand the distinct parts of the brain and how it functions normally. The average human brain weighs around three pounds and is an essential organ in the human body. The brain is responsible for all bodily functions, our intelligence and behaviour. Although the brain has many parts that all have their own functions, they all work together. The human brain is made up of three basic parts, the forebrain, midbrain, and hindbrain.
The hindbrain is located in the back, lower part of the brain and includes the upper part of the spinal cord, brain stem and the cerebellum. This part of the brain controls our bodies vital functions such as breathing and our heart. The cerebellum controls our coordinated movements and is responsible for learned motor function, for instance when you kick a ball, write, or ride a bike your cerebellum makes these things possible. And the midbrain is responsible for some of our reflex movements and plays a part in controlling eye movement and voluntary motor functions, the midbrain also contains the upper part of the brainstem. The forebrain is the largest part of the human brain and primarily consists of the cerebrum, the cerebrum is responsible for our memories, conscious thoughts and actions, its this part of the brain that allows us to imagine, plan and think and it also allows us to read, play games and recognise people, places and objects.
The cerebrum is split into two distinctive parts (hemispheres), these two hemispheres ‘talk’ to each other through a thick tract of nerve fibres called the corpus callosum and, although the hemispheres appear to be mirror images of each other they have vastly contrasting functions. For instance, the right-side hemisphere controls our ability to recognise faces, expressing emotions and primarily controls the left-hand side of our body’s movements, whereas the left hemisphere controls speech production, logical thinking, and controls movements on the right-hand side of the body. Nearly all of our bodily functions and movements are controlled by the opposite side of the brain so if a person has damage to the right-hand side of their brain, they will have impairments on the left hand-side of their body, and vice a versa.
There is a thick layer of tissue which covers the surface of the cerebrum and cerebellum called the cerebral cortex, most commonly known as grey matter. The grey matter is responsible for most information processing in the brain and has a large surface area and volume due to its many folds.
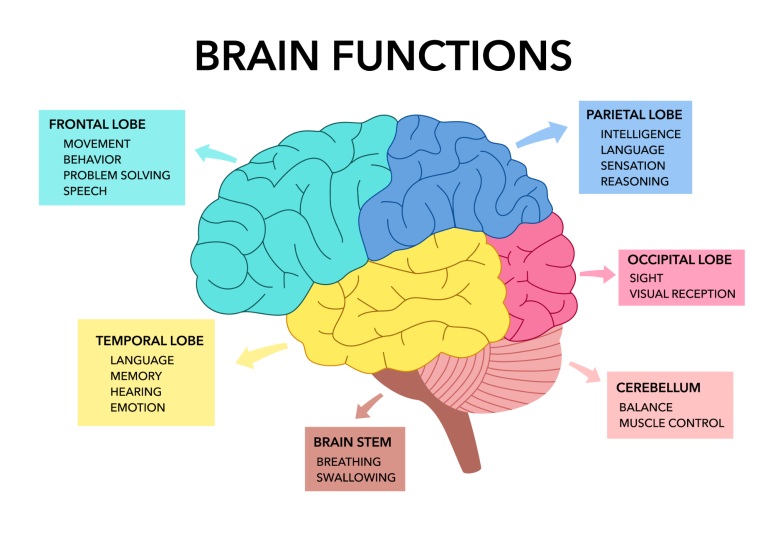
Each of the brain’s hemispheres are divided into different sections, each with its own distinctive function, these sections are called the cerebral hemispheres. We have two frontal lobes which are located directly behind the forehead and are responsible for short-term memory. The motor cortex can be found at the back of the frontal lobes, this hemisphere is responsible for executive motor functions like voluntarily moving your arms, legs, feet, and hands.
When you taste, smell or touch something your parietal lobes enable you to process these senses and are also responsible for enabling us to conduct arithmetic and reading. The somatosensory cortex receives and processes information such as touch, taste, and movements from the rest of the body, for example when you touch something that is hot or cold its this part of the brain that is recognising the temperature you are feeling. As the name suggests the occipital lobes are responsible for processing visual information. The final lobe in our brain is the temporal lobe, this part of the brain is responsible for processing information from our ears, with the underside of this lobe being where we store, form and retrieve memories from.
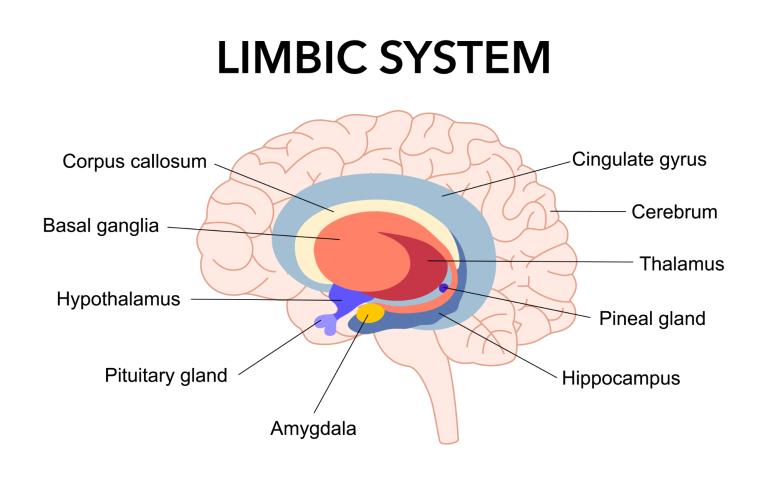
The inner brain, which is hidden from view is where the hypothalamus, thalamus, hippocampus, and basal ganglia are located and just like the cerebral hemisphere lobes each of these structures come in pairs, duplicated in the opposite side of the brain. The hypothalamus is only about the same size of a pearl, even though its small in size it plays a crucial role with many functions such as adrenaline release, waking us up in the morning and controls our emotional chemicals.
The thalamus is used by our brain to receive and direct sensory and motor information and plays a crucial role in learning, memory, sleep, consciousness, and wakefulness. A tract of nerve cells leads from the hypothalamus and the thalamus to the hippocampus which sends our stored memories to the relevant cerebral hemisphere for long-term storage and retrieving them when needed. The basal ganglia is a cluster of nerve cells that surround the thalamus, they are responsible for initiating movements.
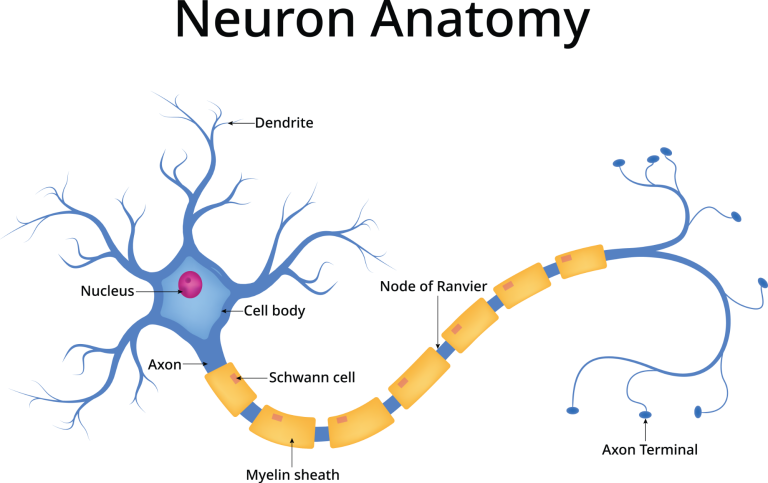
Our brain and nervous system are made up of many diverse types of cells, the primary cell is called a neuron. Every single memory, thought, feeling and movement we experience are a result of signals that pass-through neurons. There are three parts to a neuron, the cell body, dendrites, and axon.
Most of the molecules that a neuron needs to function are contained in the cell body, the dendrites extend from the cell body similar to branches of a tree and they receive messages from other nerve cells which then pass through the cell body and travel away from the cell body down an axon to another neuron, cell in some other neuron or to a muscle cell. Neuron cells are typically surrounded by many support cells; some are called a myelin sheath which wrap around the axon to insulate it. Myelin is a fatty molecule that not only insulates the axon, but it also assists with the travel of nerve signals faster and further.
Synapse is a type of junction in our brain and nervous system where a signal from a neuron passes to another type of cell, when a signal reaches the end of the axon a tiny sac called a vesicles is released, neurotransmitters are chemicals that are released by these vesicles into the synaptic cleft. These neurotransmitters cross the synapse and attach to receptors on neighbouring cells, if the receiving cell is a neuron, then the signal continues to transmit to the next cell.
Neurotransmitters are chemicals that the brain cells use to talk to each other, some make cells more active (excitatory), and others block or reduce cells activity (inhibitory). Two commonly known neurotransmitters are serotonin and dopamine, serotonin is involved in temperature regulation, constricting blood vessels and inducing sleep, low levels can cause problems with sleep, depression but elevated levels can lead to seizures. Dopamine can excitatory or inhibitory mood and complex movements, many medications used to treat mental health disorders work by modifying dopamine in the brain.
CTE, chronic traumatic encephalopathy is no ‘new’ disease, it was first documented in 1928 in boxers, but was called ‘punch drunk’ (Martland,1928). CTE is now known to be a progressive neurodegenerative disease that was first thought to be caused by concussions and traumatic brain injuries but recent studies have shown that CTE has been found in athletes, military personnel, victims of domestic violence and other patients with a history of repetitive head trauma who have never had a documented concussion, this has led to scientists now believing that CTE is not just caused by concussions and traumatic brain injuries (TBI) but also by repetitive mild traumatic brain injuries, also known as asymptomatic sub concussive hits. This accumulative trauma to the brain causes an abnormal build -up of Tau. Repeated trauma to the brain through concussions and sub-concussive impacts can result in the breakdown of the tau microtubule which can in turn lead to release of tau proteins (Gerges,2023).
You have probably heard that Tau build -up is common in some forms of dementia, but what is Tau? Tau is a type of protein that is found in the brain, and it plays a crucial role. Tau is a protein found in neurons in the nervous system and is used in the brain to stabilise microtubules, which are rigid hollow tubes that are responsible for the transport of molecules and nutrients within our brain’s neurons. In some types of dementia and CTE these tau proteins detach from the microtubes, they become modified into abnormal shapes and form ‘clumps’ called neurofibrillary tangles (NFT). These ‘tangles’ disrupt our brains neuron functions and ultimately, causes cognitive decline. These ‘mutated’ tau proteins are called p-tau.
Another change that happens to the brain after trauma is that neuropil threads develop, these microscopic ‘threads’ are abnormal structures in the brain, found in the parts of the brain that contains neuron processes and synapses, usually within the grey matter part of the brain. They occur when the tau protein undergoes a mutation which changes the proteins activity, structure and interactions with other molecules which causes an excessive amount of tau to build up.
The pattern of Tau protein build-up in the brain of someone who has CTE is distinctively different to someone who has a different neurodegenerative disease such as Alzheimer’s, typically ‘spaces will appear in the brains white matter, particularly in the temporal lobe. In later stages of CTE macroscopic changes can occur such as grey and white matter atrophy, reduction in brain weight, atrophy in the thalamus, hypothalamus, and mammillary bodies In the mildest stages of CTE it is typically seen that there is a deposition of p-tau protein in clusters in the neocortex, often arranged along the small blood vessels, extending from the surface of the brain to the lowest parts of the grey matter which affect the neurons. This type of p-tau protein build-up has not been observed in a person who has not been exposed to some type of repetitive brain trauma (McKee,2015).
Mckee and her colleagues published a staging of pathology in CTE in 2013 and later again in 2018 with four stages (stages I-IV). Stage I will have isolated p-tau lesions in the cerebral cortex, stage II will have multiple p-tau in the cerebral cortex, particularly in the frontal, temporal, and parietal lobes with the NFTs being scattered throughout the cerebral layers. Stage III will display degeneration in the medial temporal lobe, affecting the hippocampus, entorhinal cortex and amygdala, as well as p-tau located around blood vessels, the most severe stage of CTE, stage IV there will be severe p-tau throughout the cerebrum, medial temporal lobe structures, brainstem, cerebellum and sometimes seen in the spinal cord.(McKee,2018).
Studies carried out by McKee and her team have shown that the average onset of CTE in athletes symptoms occurs 14.5 years after retiring from their sport (McKee,2013) with severity in symptoms and stage of CTE being in direct relationship with the number of years that the patient has been exposed to TBIs or/and sub-concussive hits.
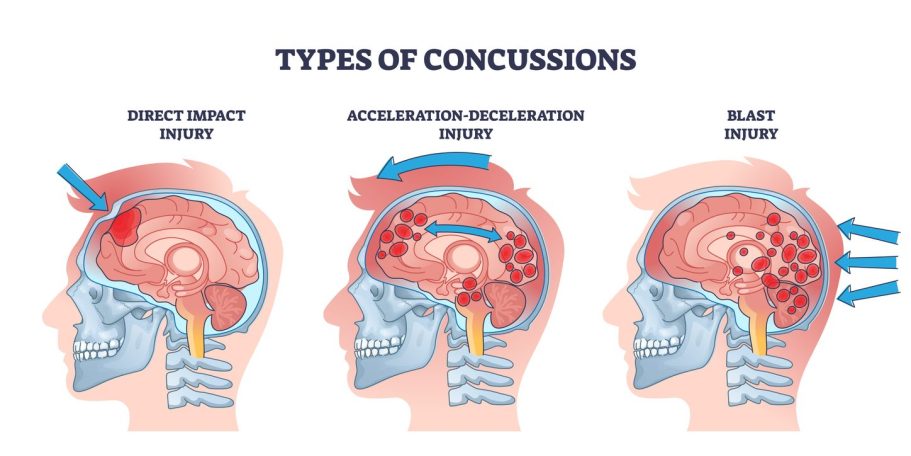
What is meant by a sub-concussive hit? These are typically experienced in contact sports such as rugby, when a person is exposed to either a direct or indirect impact to the head that does not cause a concussion or TBI, and usually shows no symptoms at the time. The impact to the brain or body causes the brain to impact the inside of the skull and can also cause the brain to twist within the skull, similar to what happens to the brain during a car crash. These movements, impacts and twisting motions cause harmful inflammation and even microscopic tears, it is estimated that that a rugby player will experience in excess of over 1500 sub-concussive hits per typical season, whereas a football player can experience up to 1400 sub-concussive hits per season, depending on how many times they header the ball.
Another cause for concern with sub-concussive hits is the damage these types of brain trauma have on the blood-brain barrier (BBB). The brains BBB is made up of a complex network of capillary cells with tight junctions and astrocytes that provide the link between cells and neurons. A study conducted by Marchi in 2013 looked at the brains of American football players who had no reported concussions, after one season medical imaging showed evidence of BBB disruption (Marchi,2013)
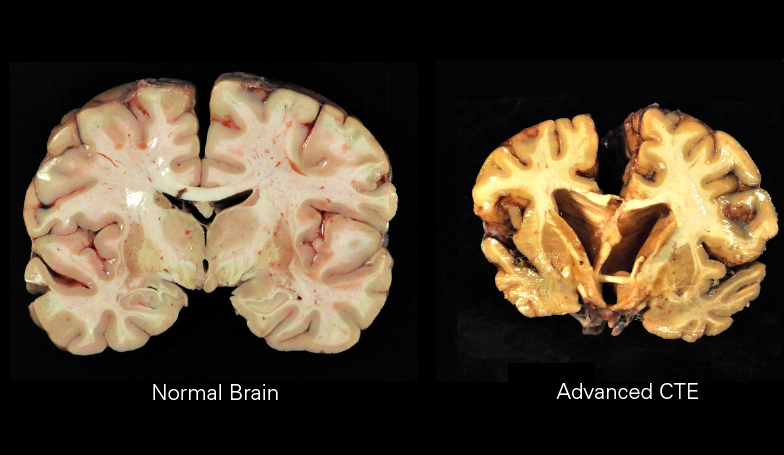
Currently there is no definitive way to diagnose a living person with CTE, due to the fact no scan or other type of test is able to show the characteristic brain damage and p-tau deposits that define CTE, these telltale signs of CTE can only been seen by examining the brain tissue under a microscope. However, the National Institute of Neurological disorders and Stroke (NNDS) have recently published their criteria for the diagnosis of traumatic encephalopathy syndrome (TES), the purpose of which is only to be used in the research of CTE. According to this research diagnostic criteria guidelines is to establish the likelihood that a patient has CTE, which would then be confirmed or dismissed after death by examining their brain. This tool will most likely play a significant role into the research being conducted to enable doctors to diagnose CTE in a living person. The diagnosis of TES requires 4 important factors, that the patient has experienced substantial exposure to repetitive head injuries (RHIs), they display core clinical features of cognitive impairment and/or behavioural dysregulation, their symptoms are on a progressive course and that all their clinical symptoms are not fully accountable by any other neurological, psychiatric or medical conditions. The patient’s functional dependence will be graded on five levels, ranging from being independent to severe dementia (Katz ,2021).
By understanding how the brain works and what effect concussions and sub-concussive impacts have on the brain its not hard to understand why patients with probable CTE display such a wide range of symptoms which can affect many different parts of their brain and body and can vary in severity from one patient to the next.
It’s mind boggling how sporting bodies continue to attempt to discredit the mountain of scientific data that proves the serious long-term health risks to athletes brains who take part in contact sports, our aim at Marshalling CTE is to raise awareness of these known risks so that the public can make informed choices and we urge anyone who has a history of any type of brain trauma and are experiencing CTE symptoms to seek medical advice and make sure that their doctor is aware of their brain trauma history.
The symptoms of CTE are linked to the distinct stages of the disease, McKee classified these symptoms against her pathological stages of CTE. Stage I being asymptomatic or mild memory and depression symptoms, stage II displaying symptoms including behavioural outburst and severe depression, stage III will display symptoms of cognitive deficits including memory loss and problems with executive dysfunction and stage IV will experience advanced language deficits, psychotic deficits, and motor features (McKee,2013).
References (in chronological order):
Martland HS. Punch drunk. JAMA. 1928
N. Marchi, J.J. Bazarian, V. Puvenna, M. Janigro, C. Ghosh, J. Zhong, T. Zhu, E. Blackman, D. Stewart, J. Ellis. Consequences of repeated blood–brain barrier disruption in football players. PLoS ONE 8: e56805. 2013
A.C. McKee, R.A. Stern, C.J. Nowinski, T.D. Stein, V.E. Alvarez, D.H. Daneshvar, et al. The spectrum of disease in chronic traumatic encephalopathy. The National Library of Medicine.. (2013)
A.C McKee, T Stein, P Kiernan, V Alvarez. The Neuropathology of chronic traumatic encephalopathy. The national Library of Medicine. 2015
A.C. McKee, J. Kriegel, Z Papadopoulos. Chronic Traumatic Encephalopathy: Is Latency in Symptom Onset Explained by Tau Propagation?. The National library of medicine. 2018
D. Katz , AC Mckee, et al. National Institute of Neurological Disorders and Stroke Consensus Diagnostic Criteria for Traumatic Encephalopathy Syndrome. The National Library of Medicine. 2021
J A. Gerges, I. Chalhoub, C. Atallah, R. Khoury. Biomarkers of chronic traumatic encephalopathy: A state-of-the art review. Biomarkers in Neuropsychiatry.2023
Are you experiencing a mental health crisis?
There is help for you!
Shout: For 24/7 text support, text SHOUT to 85258 or click HERE
NHS 111 Online or Phone: If it's not an emergency but you need urgent help with your mental health, you can access NHS 111 online or by calling 111
Samaritans: Call 116 123 to talk , or email: jo@samaritans.org for a reply within 24 hours or click HERE
CALM - 0800 585 858 or click HERE
Mind - 0300 1233 393 or click HERE
No Panic - 0844 9674 848 or click HERE
National Domestic Abuse - 0808 2000 247 or click HERE